How AI Could End the Dangerous Cycle of Symptom Rationalization in the Medical Community
“Human beings are not rational, but rationalizing animals”, Neel Burton M.D tells us. “If they find it frightening to think and painful to change, this is in large part because thinking and changing represent major threats to the beliefs that make up their sense of self”. This insight rings especially true with healthcare workers who base their identities on assuming the role of caregiver. For many physicians the acknowledgment of a more serious health condition is extremely difficult because doing so challenges their perception of self.


How AI Could End the Dangerous Cycle of Symptom Rationalization in the Medical Community
They say never trust a skinny chef, but what about an unhealthy doctor? As doctors we spend our days extolling the benefits of regular healthcare and modern medicine, yet all too often when it comes to our own health we don’t practice what we preach. Last week we covered physician depression, why it often goes undiagnosed, and how one day AI could offer a solution. This week, we pivot from mental health to physical health, investigating why many healthcare experts don’t place importance on their personal well-being, and how developments in Artificial Intelligence could hold the key to aiding doctors in improving not just their patients health, but their own health as well.
Everyday we implore our patients to follow our recommended care regimens, and attempt to reason with the ones who, for reasons unknown to us, simply won’t. We get frustrated when patients brush off years of evidence-based medicine claiming they know better, but in reality are we any different? In an article titled, Doctors as patients: a systematic review of doctors' health access and the barriers they experience, researchers found that “ two-thirds of the physicians do not have a regular family physician, and physicians who suffer from chronic diseases are even less likely to be treated than the healthy ones”. As the sector of the population who arguably is most aware of the consequences of poor healthcare, why are we not prioritizing our own?
You’ve heard the old adage a lawyer who represents himself has a fool for a client, but what about the doctor who treats themselves? In a study on doctor’s health-seeking behavior 90% of physicians surveyed believed it was acceptable to self-treat minor or acute conditions, whereas only 25% felt the same way about more serious or chronic conditions. On the surface this seems logical. We didn’t suffer through medical school to not be able to treat our own common cold, but where do you draw the line between a minor illness and something more serious? We’d all like to think we are capable of using good judgment when it comes to our own health, but self-treatment can be a slippery slope. 70% of doctors report that they would only see a doctor if they were seriously ill, but as the article Doctors as patients: a systematic review of doctors' health access and the barriers they experience states, “Medical knowledge enables doctors to justify their symptoms as ‘insignificant’. When doctors' reluctance to seek health care for minor illness is coupled with this tendency to rationalise symptoms as minor conditions, the potential seriousness of this barrier is recognised”.
“Human beings are not rational, but rationalizing animals”, Neel Burton M.D tells us. “If they find it frightening to think and painful to change, this is in large part because thinking and changing represent major threats to the beliefs that make up their sense of self”. This insight rings especially true with healthcare workers who base their identities on assuming the role of caregiver. For many physicians the acknowledgment of a more serious health condition is extremely difficult because doing so challenges their perception of self. Uncomfortable with relinquishing control to assume the role of patient, and operating on the belief that trained medical professionals need only seek care for “serious issues”, doctors fall into a dangerous cycle of symptom rationalization. More often than not, the only catalyst strong enough to disrupt this pattern is when symptoms reach a level of severity so unmistakable the physician is forced to confront the reality of their situation. Unfortunately, at that point it may be too late.
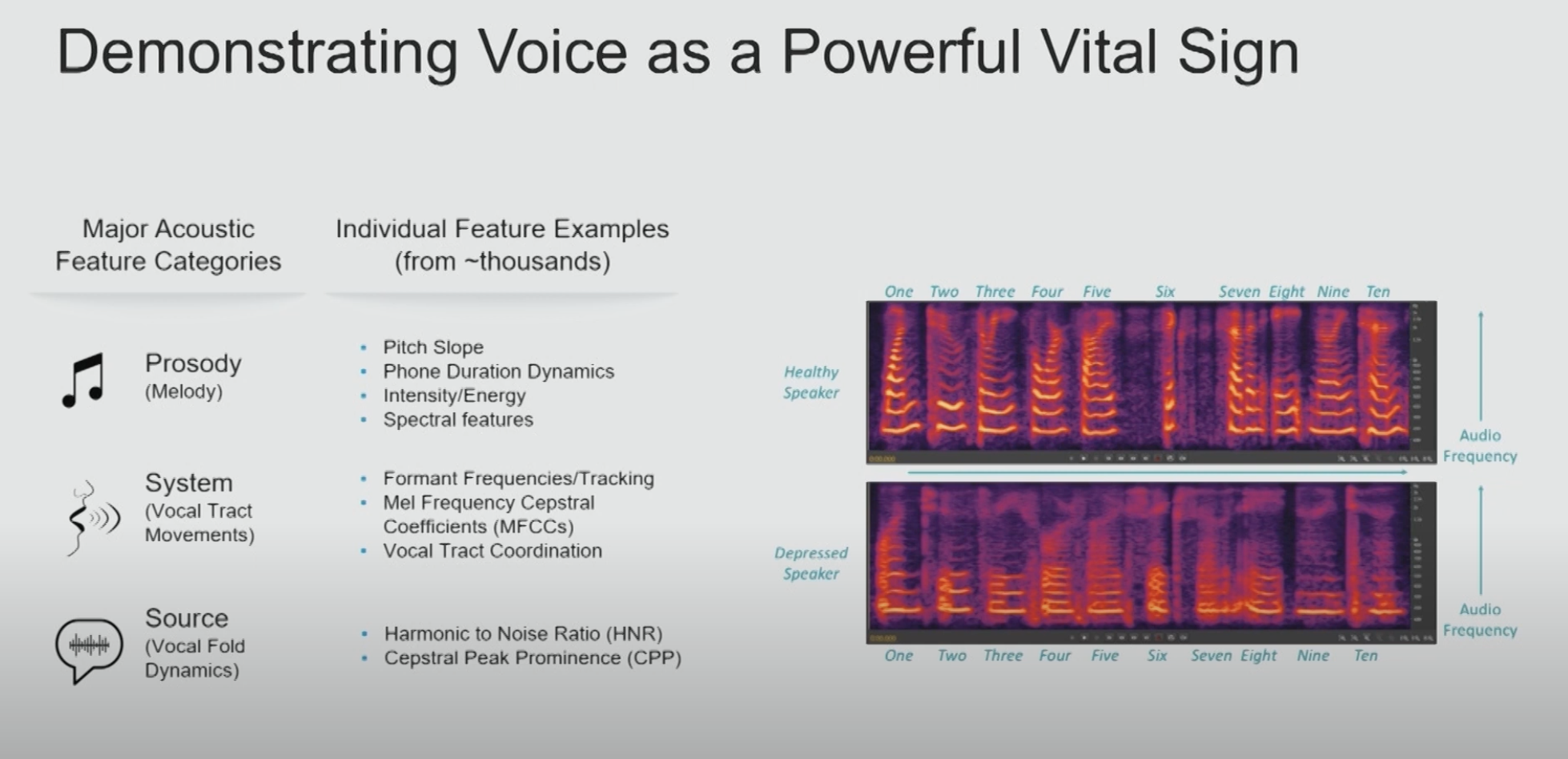
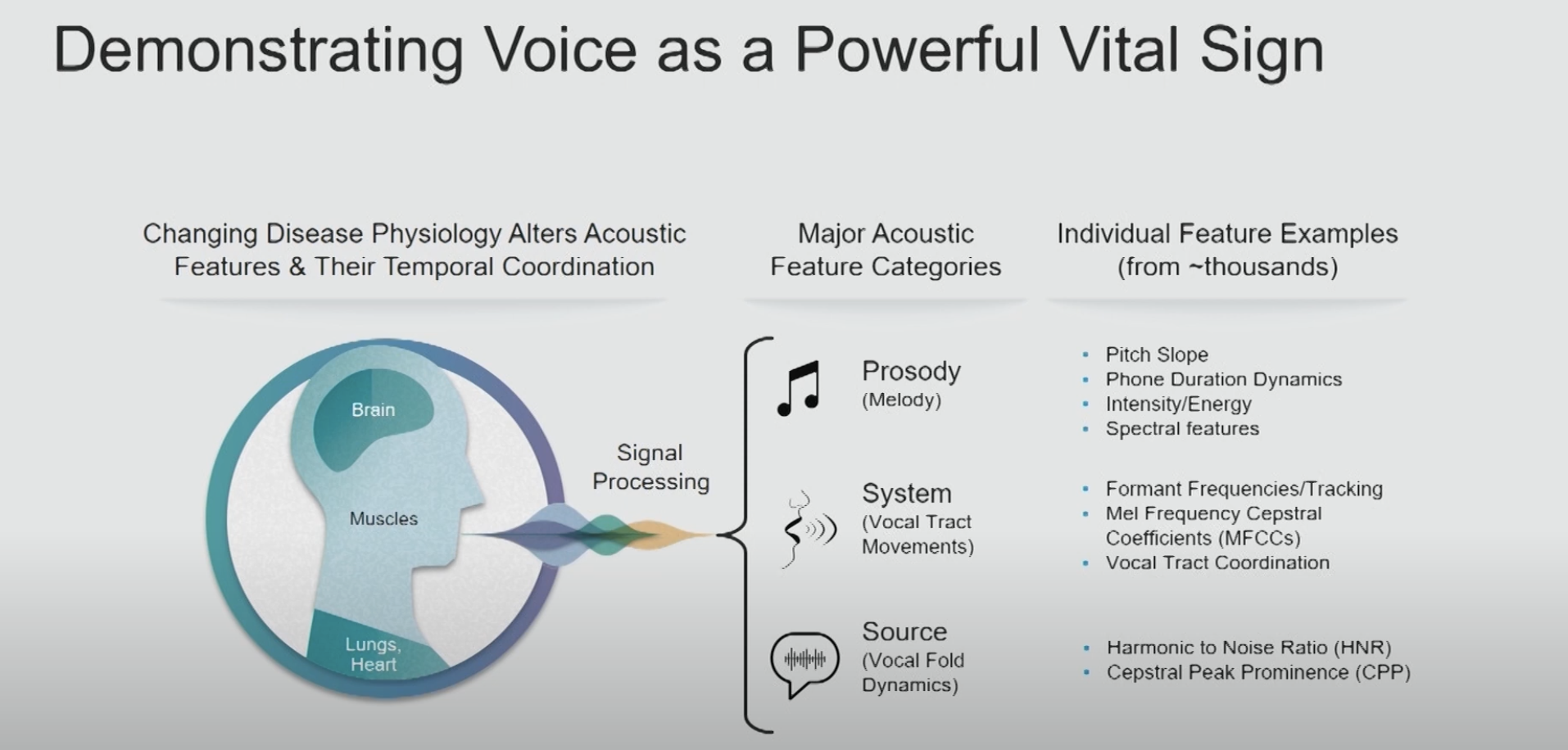
Symptom rationalization is essentially self-deception making it an especially difficult issue to combat because. Physicians engaging in symptom rationalization truly believe they are in good health, and therefore do not pay heed to materials on self care or provider well-being as they do not think them pertinent to their situation. Rather than focusing efforts on changing those who see no issue, Artificial Intelligence may offer an alternative solution free from the humanly toils of self identity and worth. In past articles we covered how AI is being used to detect vocal biomarkers in voice which indicate the presence of a variety of health conditions such as coronary artery disease, pulmonary disease, congestive heart failure, and sleep apnea, and dementia.
We know that one day AI Scribes will become a staple in every exam room. As AI Scribes monitor doctor-patient conversations, they will be able to detect vocal anomalies not just in patients, but in their physicians as well. With the majority of symptoms having multiple potential causes, the current state of disease diagnosis is certainly not an exact science which leaves ample room for plausible deniability when it comes to physician health concerns. Vocal biomarkers map to specific conditions with a high level of precision and accuracy leaving no room for guesswork or debate. This could provide life-saving early detection for many diseases, ending the cycle of clinician's rationalizing away their symptoms to avoid getting care. While these developments are still in early stages, we are hopeful that AI might hold the key to unlocking a healthier future for those who have devoted their lives to the health of others.
text
Related Stories
Realize the full potential of Healthcare AI with DeepScribe
Explore how DeepScribe’s customizable ambient AI platform can help you save time, improve patient care, and maximize revenue.